The idea of extracting a malignant glioma from the cranium through an incision the diameter of a pencil would probably have been laughed off as a strange thought a few years back. Equally strange would have been the thought of surgery performed by robots with commands from surgeons. These are now far from being figments of the imagination.
Advances in surgical technologies along with the marriage of optoelectronics, digital technologies and robotics with traditional surgical process have enabled less traumatic and more efficient procedures. The progress of modern surgical technology has been fast paced, with innovative techniques taking the place of traditional methodologies. The most obvious leap, however, has been the reduction of invasion in surgical procedures.
FROM DIAGNOSIS TO SURGERY
Traditional surgery involves the exposure of the entire operating area, thereby increasing the visibility and ease of intervention. The associated risks of infection, blood loss and postoperative complications are high. Patient discomfort owing to trauma of the adjacent soft tissue also led medical researchers to come up with techniques to minimise the risks associated with traditional surgery.
Minimally Invasive (MI) surgical interventions make use of scopes. The surgery is done through minimal incisions just big enough to allow entry. Such incisions are called ports and the technique is called port-access surgery.
See Also:
The scopes have an eyepiece, which enables the surgeon to visualise the interior of the body. Tiny cameras attached to the eyepiece allow more than one observer to view the operating field.
How well do you really know your competitors?
Access the most comprehensive Company Profiles on the market, powered by GlobalData. Save hours of research. Gain competitive edge.

Thank you!
Your download email will arrive shortly
Not ready to buy yet? Download a free sample
We are confident about the unique quality of our Company Profiles. However, we want you to make the most beneficial decision for your business, so we offer a free sample that you can download by submitting the below form
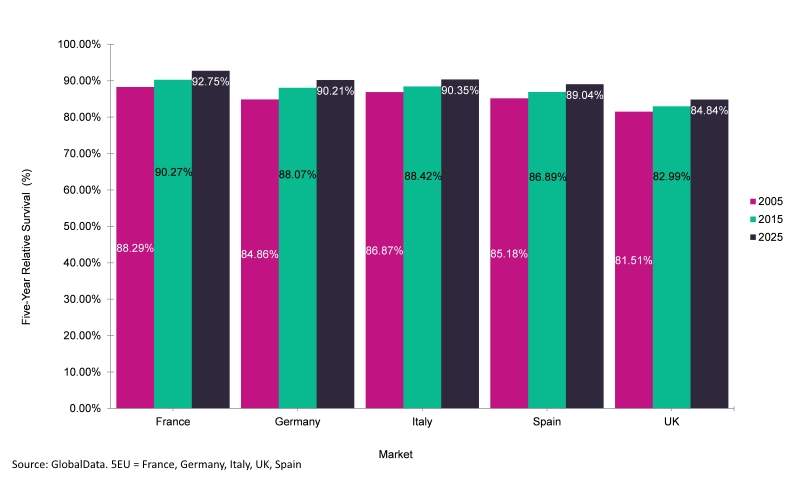
By GlobalDataIn addition to clinical outcomes, there are several financial benefits associated with this technique, such as shorter hospital stays, which are especially important in public-funded healthcare systems such as those in Europe.
CLINICAL UPTAKE OF MI
The levels of penetration of MI techniques into various clinical specialities cannot be surmised, owing to the differences in complexities involved in performing the surgery at different sites. The limited manoeuvrability of the instruments through the small operative area is often considered a detriment in expanding the application base of this method.
Nevertheless there has been an upsurge in the levels of adoption with miniaturisation of instruments and technology developments that aid in better visualisation of the operating area. The size of the access ports has shrunk from 10mm to 2mm giving rise to the concept of needlescopic ports.
Since the 1970s there has been extravagant use of MI surgery in certain areas of general surgery such as cholecystectomy. Over 90% of routine cholecystectomic procedures are performed laparoscopically.
The use of MI techniques, such as disc nucleoplasty, in the correction of arthritis, is on the rise. The accession into narrow lumen areas such as the arteries and the cerebrovascular system limited the use of minimal access surgery until recently. With the emergence of robotic surgery there are more surgeries being performed in these areas.
The presence of such high-precision instruments, coupled with superior visualising capabilities, has increased the uptake of this technique in areas such as coronary artery bypass graft, endoscopic sinus surgery and disc nucleoplasty, to name a few.
IMAGE-GUIDED SURGERY
In the age before Image-Guided Surgery (IGS) systems came into the picture, surgeons could only view anatomical surfaces during MI surgery using endoscopes. Determination of structures outside this vision was wholly dependent on the surgeon’s knowledge and skill. Now, a combination of tracking technology, special software, position measurement systems and high-speed computing has produced systems that can display on screen, and in real time, the movement of surgical instruments in the patient’s anatomy.
Such navigation enables a better view of the surgeon’s instruments in the context of the patient’s body, making the procedure far more accurate. Such accuracy also ensures that the damage to healthy tissues can be minimised. The benefits of IGS include improved surgical outcomes, shorter operation time, less invasion into the body, quicker recovery time and cost-efficiency in existing procedures.
The concept of image guidance has also spurred shift in the focus of medical imaging. Imaging has moved from the area of diagnosis to the arena of treatment.
The promise of IGS has been largely realised in neurosurgery, where it is in widespread use. The applications of IGS are diverse. From a more or less mature neurosurgery market to spinal, ENT, dental and the promising orthopaedic surgery market, IGS is fast expanding its scope.
In orthopaedic surgery IGS is used for improving implant positioning, balancing and alignment to increase the lifetime of implants and provide the patient with better mobility and greater comfort.
IGS SYSTEMS AND APPLICATIONS
The IGS system comprises a tracking device or a camera, a registration device that can align preoperative images with the real-time patient image and other components. The systems may vary with the incorporated technology, module structure and their compatibility with different existing modalities. Some of the current modalities include fluoroscopy-based models, CT-based models and models based on electromagnetic or optical cameras.
Another application of image guidance is Gamma Knife stereotatic radio surgery, where a highly precise and focused dose of radiation is delivered to specific areas in the brain to destroy tumours or vascular malformations. Research and studies are underway to enable precise and targeted chemotherapy drug delivery using catheters placed on the site from where the tumour has been removed to kill any remaining cancerous cells. This way the effect of these drugs on healthy cells is minimised.
The application focus of IGS is developing not only in MI surgery, as was originally intended, but also in open surgeries. When used in interventional applications, it often leads to a blur between medical specialities. Hospitals and healthcare organisations will have to adapt to this change and choose where to apply the technology most effectively.
MINIMAL SURGEON PRESENCE
The advancement of technology has always been an attempt to improve present conditions. This would definitely be applicable to surgical technology. Open surgery evolved into MI surgery and now minimal-surgeon-presence surgery. The transition has already begun, with voice-assisted robotic surgeries being practised the world over.
The use of robots in surgery has opened up an entire field for surgeons to explore and master. The dexterity built in a robotic system can ensure that the surgery is performed with utmost precision. However such systems are very expensive and this poses a severe limitation on their widespread use.
Robot-assisted surgery has opened up a new branch of telesurgery. In conjunction with IGS, the possibilities of robotic surgery in both on-site and telesurgery are immense and are just starting to be explored. This has the potential to become the preferred way of surgery in the future, as the expertise of surgeons from across the world can be gathered in one operating room with the help of telecommunications and powerful internet capabilities.